A new research carried out by Dr. Bruce T. Lamb from the Department of Neurosciences at the Cleveland Clinic, reveals more details about the link between the immune system and neurodegenerative diseases like Alzheimer's, associated with high accumulations of tau protein.
The tau protein is found inside neurons and its function is almost like that of a skeleton, providing support and framework for the cell.
The problem is that when abnormal tau appears, it gathers into filamentous deposits that are damaging for neurons.
Previous research established that groups of microtubule associated protein tau, or MAPT, with several phosphate groups linked, are a main feature of neurodegenerative disorders (tauopathies), like Alzheimer's or other dementia.
In order to prove that cells which normally help the central nervous system can also trigger pathological changes in the brain, Dr Lamb carried out an experiment that examined the link between microglia (cells that play an important role in the immunity of the nervous system) and tauopathy.
He looked at a specific signaling pathway that allows neurons and microglia to communicate, called fractalkine (CX3CL1) – a chemokine expressed in neurons, and its receptor (CX3CR1) which is only expressed in microglia.
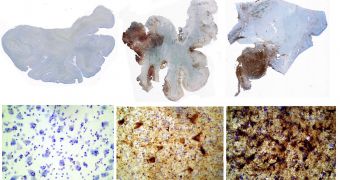
Lamb assessed changes in this signaling pathway in several mouse models, including a model of tauopathy (hTau) a model of inflammation and microglia and neurons grown in the lab.
The results showed that inflammation caused by microglia favored MAPT phosphorylation and aggregation in all of the experimental models.
He said that “importantly, introduction of CX3CR1 deficiency into hTau mice resulted in altered microglial activation, enhanced MAPT phosphorylation and aggregation, as well as behavioral abnormalities.
Previous research suggested a link between inflammation in the nervous system and the tauopathies, but Dr Lamb said that “there is little mechanistic evidence that altered microglial activation plays a pathogenic role in the formation of MAPT pathologies.”
Besides observing the effects of a specific microglial receptor on MAPT pathology, the study also allowed a better understanding of the specific signaling molecules downstream of the CX3CL1/CX3CR1 interaction.
The results of this research suggest that there is hope for a potential therapeutic strategy for tauopathies, as they are increasing neurodegenerative disease, that affect over 5 million people in the US with AD and several other millions affected by non-AD tauopathies.
This new research was published by Cell Press in the October 7th issue of the journal Neuron.
 14 DAY TRIAL //
14 DAY TRIAL //