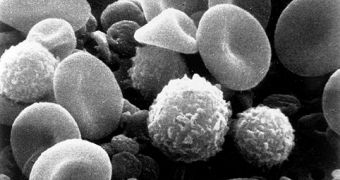
After about 50 mouse studies, experts at the Johns Hopkins University (JHU) have managed to finally map the complete set of actions that a certain set of white blood cells takes when dealing with badly damaged lungs. According to the investigations, these regulatory T cells, or Tregs for short, are the main triggers that set the pace of the recovery, depending on the seriousness of the injury or damage. The only thing experts knew for sure about them was that they played a crucial role in keeping the immune system away from healthy tissues, e! Science News reports.
“Our study results are the critical first leads in finding treatments for a clinical condition that until now has had none, despite its high mortality,” JHU pulmonologist Landon King, M.D., who has also been the senior investigator of the new study, explains. “When a patient develops acute lung injury, we want the critical care medicine team to be able to do more than just stabilize the patient on a ventilator,” he says. King is also the JHU School of Medicine director of pulmonary and critical care medicine. Details of the research appear in the September 21st online issue of the Journal of Clinical Investigation.
The new study is groundbreaking in many ways, and could open up entirely new fields of drug synthesis. For example, therapies could be devised that would essentially supplement levels of Tregs in people who are lymphocyte-deficient on account of chemotherapy or lung diseases. Other drugs could be designed to be used to speed up the activation of these white blood cells after an injury, so that the immune system goes to work right away, rather than wasting precious and often-critical time. According to statistics, more than 200,000 US citizens suffer some form of sudden, acute lung injury.
“T cells and the body's active immune system play a crucial role in recovery from acute lung injury. It is by no means a passive process as previously thought,” JHU Bayview Medical Center pulmonologist and instructor Franco D'Alessio, M.D, says. His team determined the exact type of white blood cells that played the most important role in the healing process. He noticed that one subset of the CD4 T lymphocytes, technically known as CD4+ CD25+ Foxp3+, or regulatory T cells, was present at the injury site since day one, and spiked at day seven, remaining constant until the tenth day of recovery.
“Our study should spark lung experts here and elsewhere to shift their research focus from nearly universal interest in the onset of acute lung injury to new mechanisms underlying resolution of lung injury,” King concludes.
 14 DAY TRIAL //
14 DAY TRIAL //