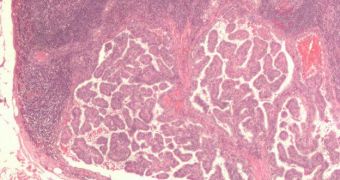
A large portion of people who lose their lives after developing melanoma do so because of metastasis, which is the generalized spread of cancer to all major organs. Yale University investigators have recently found a new biomarker that can predict which melanoma patients are at risk of metastasis.
Monitoring melanoma currently required the use of advanced, and therefore costly, medical imaging methods. As such, the development of a new diagnostics tool could go a long way towards improving melanoma survival rates, experts believe.
In the new study, experts discovered a set of plasma biomarkers that provide a fairly good assessment of which melanoma patients will go on to develop metastasis. Details of the work appear in the latest issue of the journal Clinical Cancer Research.
The magazine is edited by the American Association for Cancer Research (AACR). Official statistics show that melanoma is the 5th most common cancer in men, and the 7th most common in women.
Of the 68,130 people that were diagnosed with this form of cancer in the United States in 2010, about 8,700 died as a result. Most of these victims perished due to lack of access to proper screening methods, healthcare experts say.
When these methods are available, and are applied in time, melanoma can be treated using simple surgical procedures, through which the affected area is extracted in its entirety. Moratility rates increase only when the cancer is not detected, and is left untreated.
There are different types of melanoma, ranging from stage 1A to stage 3C, and each of them subjects people to various risks of death. Stage 1A melanoma typically involves a 10 percent mortality rate, whereas stage 3C skin cancer is deadly 70 percent of the time.
“The rate at which melanoma is increasing is dramatic, and there is a huge number of patients under surveillance,” explains Yale School of Medicine associate professor of medicine Harriet Kluger, MD.
“Our current method of surveillance includes periodic imaging, which creates huge societal costs,” the investigator adds. Some 216 people were used in the new experiments, which sought to determine the existence of previously-unknown biomarkers.
About 108 individuals in the group had been diagnosed with metastatic melanoma, whereas the other half had been found to suffer from stages 1 and 2 of the condition. The team managed to identify CEACAM, ICAM-1, osteopontin, MIA, GDF-15, TIMP-1 and S100B as biomarkers for the cancer.
“This finding will need to be confirmed prospectively before it is used in the clinic, but it shows that such testing is possible,” Kluger explains.
 14 DAY TRIAL //
14 DAY TRIAL //