A collaboration of investigators from the Massachusetts Institute of Technology, in Cambridge and Brigham and Women's Hospital has recently come up with a new therapeutic approach for addressing drug-resistant bacteria. Their method relies on the use of special nanoscale particles.
Drug resistance developed in bacteria for a large number of reasons, including the fact that people take antibiotics on their own, without consulting a doctor. They take these drugs even if they have viral, not bacterial, infections, and the habit takes its toll.
Additionally, some patients simply do not respect doctors' orders. Instead of taking the medicine they are prescribed for the length of time their physicians indicate, some people only take the drugs for half that time, until their symptoms disappear. This allows the bacteria to develop immunity to that drug.
Some time ago, experts suggested that using highly-targeted nanoparticles to impact the bacterial colonies directly could prove to be an effective method of addressing drug-resistant microorganisms.
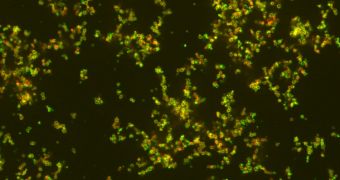
In the new study, the MIT/BWH team was able to demonstrate that such nanoparticles can be built. The structures the group produced are able to bypass the body's immune system while carrying antibiotics, arrive at the infection site, and deliver strong, undiluted dose of the medicine inside bacteria.
Advantages beyond increased drug efficiency include a reduction in the severity of adverse side effects, such as the destruction of useful bacteria in the gut. The statement was made by MIT graduate student Aleks Radovic-Moreno.
He was the lead author of a new paper describing the findings. The work appears in the latest issue of the esteemed scientific journal ACS Nano, which is published by the American Chemical Society.
The newly developed nanoparticles are also capable of delivering their payloads into bacteria colonies over prolonged periods of time, between 24 and 48 hours. This further increases the efficiency of antibiotics, while reducing the microorganisms' chances of survival.
“You don’t want just a short burst of drug, because bacteria can recover once the drug is gone. You want an extended release of drug so that bacteria are constantly being hit with high quantities of drug until they’ve been eradicated,” Radovic-Moreno concludes.
 14 DAY TRIAL //
14 DAY TRIAL //