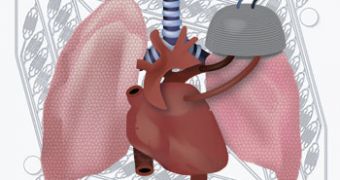
American scientists say that a technology for building artificial lungs could significantly reduce the death rate of patients waiting for a lung transplant.
Joseph Vacanti and coworkers at Massachusetts General Hospital, in Boston made a huge advancement in this field, by developing a device that is able to make the carbon dioxide-oxygen gas exchange, when implanted in the body.
This gives patients awaiting for a transplant far more freedom and a better chance of survival, RSC reports.
The researchers actually designed a microfluidic branched vascular network through which blood flows, and that is separated from a gas-filled chamber by a silicone membrane less than 10um thick.
The artificial network is build by a biocompatible polymer called polydimethylsiloxane, cast on a micro machined mold.
The most difficult thing in designing the device was getting a blood pressure within the channels, very similar to that in veins and arteries.
David Hoganson, Vacanti's coworker said that “fulfillment of these design criteria necessitated creating channels that had variable depth throughout the network and also had precise curvature.”
To do that, Vacanti's team used computational fluid dynamics and optimized the vascular network's structure so that it would avoid clotting induced by excessive blood pressure.
When the lung is severely affected, it is unable to remove carbon dioxide from the blood, thus reducing the efficiency of the oxygen uptake.
The problem today is that there are not enough donors, so patients awaiting for a transplant have very high mortality risks.
And since the only technology that can help them is found in intensive care units, the patients' quality of life is often affected.
The device developed by Vacanti and his team could be made into an implant-sized one, fabricated by “stacking the functional layers of the device to achieve the necessary surface area for gas exchange,” Hoganson said.
Anyway, Jaisree Moorthy, a specialist in using microfluidics in tissue engineering at the University of Pennsylvania, says that Vacanti's device offers a very elegant solution, since it “is more efficient due to a thinner membrane, and mimics the biological CO2/O2 transfer rate.”
 14 DAY TRIAL //
14 DAY TRIAL //