Experts recently managed to develop two new, different approaches of attacking the MRSA, and destroying it for good. Their findings could help save countless lives.
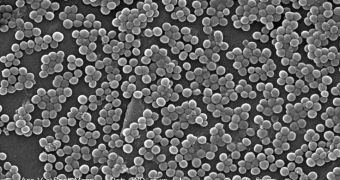
MRSA stands for methicillin-resistant Staphylococcus aureus, a bacterium that is among the leading causes of deaths from hospital infections around the world.
The microorganism can endure harsh conditions, and has over the years “learned” to adapt itself to the effects of various drugs, thus becoming immune.
It attacks mostly people with weak immune systems, including but not limited to children, the elderly, coma patients, those who just got transplants, and so on.
Generally, it infects skin, soft tissue, the bloodstream and lungs, and contracting MRSA is oftentimes fatal. Experts have been trying to discover a way of rendering it powerless for many years.
In one of the two new studies, the investigators demonstrate a way of addressing one of the key abilities the bacteria has, which is to evade the action of its host's immune system.
The other paper, published around the same time, shows a method for destroying the pathogen's tissue-damaging mechanisms, ScienceDaily reports.
The investigations, which were conducted on unsuspecting lab mice, reduced the overall virulence of the staph infection in the small rodents.
Given the similarities we share with mice, experts are hopeful that this discovery could be extended to human subjects as well. Human trials have not yet been conducted though.
“Staph aureus is the world champion of immune suppression,” says University of Chicago professor and chair of microbiology Olaf Schneewind, PhD.
“Even when the infection can be cleared with antibiotics and surgery, the patient has no immunity. So these infections often recur,” adds the expert, who is the senior author of both research papers.
The two studies were funded with grant money secured from the US National Institutes of Health (NIH) and Novartis Vaccines and Diagnostics.
Additional contributors included UM students and Indiana University School of Medicine-Northwest expert Taeok Bae, ScienceDaily reports.
 14 DAY TRIAL //
14 DAY TRIAL //