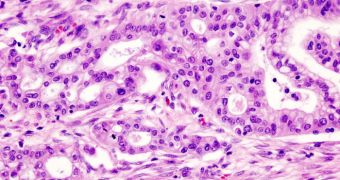
American investigators have determined that the vaccinia virus construct GLV-1h153 – a genetically engineered viral agent – holds great promise for imaging and treating pancreatic tumors, one of the most dangerous forms of cancer.
What makes this new lead so promising is the fact that it could allow oncologists to check on the progress the virus is making against pancreatic cells in a non-invasive manner. At this time, doctors need to collect biopsies in order to assess the efficiency of their medication plans.
The new virus was carefully developed by experts at the Memorial Sloan-Kettering Cancer Center, in New York, who collaborated closely with colleagues from the San Diego, California-based Genelux Corporation. GLV-1h153 is the result of their joint efforts.
This agent was specifically engineered to encode for the human sodium iodide symporter gene (hNIS), but it can also be used for targeted radiotherapy. The noninvasive monitoring capabilities it provides can be used in the long run, without the need to inject additional amounts of the virus very often.
Experts behind the new work suggest that the agent could become the target of advanced medical imaging technologies such as positron emission tomography (PET). This would allow oncologists to assess the efficiency of their selected treatments nearly in real-time.
Details of the virus were presented at the second International Conference on Frontiers in Basic Cancer Research, which the American Association for Cancer Research (AACR) organized in San Francisco, California, between September 14-18.
Former MSKCC postdoctoral researcher Dana Haddad, MD, PhD – who is now a resident at the Mayo Clinic – explained to attendants that the viral agent was used to treat a sample of 50 lab mice that suffered from pancreatic cancer.
“We expected that we would be able to noninvasively detect virus replication in tumors using this imaging system, but we could not predict the timing of this, how long we could repeat serial imaging and whether this would actually provide information about therapeutic response,” Haddad explained.
Initially, the team was disappointed when the combination of GLV-1h153 and radioiodine (131I) began to fade from PET monitors within two weeks of injection. “When the tumor began to die due to the effects of the virus, the PET signal began to decrease,” the expert said.
“We were further pleased to observe that although tumor kill with a very low dose of virus was not very impressive, we could achieve potent tumor kill when we combined virus treatment with systemic radiotherapy,” she told the meeting.
“Using lower doses of virus and radiotherapy could minimize potential toxicity and side effects associated with both treatments,” Haddad concludes.
 14 DAY TRIAL //
14 DAY TRIAL //