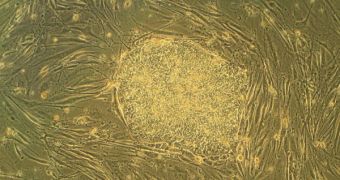
Experts at the Tufts University have recently announced in the advanced issue of the journal Tissue Engineering Part A that they managed to harness the pluripotency trait of human embryonic stem cells (hESC) in order to create complex, multi-layered, skin-like tissue. The resulting product is also similar in many ways to the oral mucosa, which is the tissue that lines the inside of the human mouth. The accomplishment goes to show the power that stem cells have in differentiating into any type of cell, and offers a glimpse at future applications for hESC.
The research team was composed of Tufts University School of Dental Medicine (SDM) experts, working together with colleagues from the University's Sackler School of Graduate Biomedical Sciences (SSGBS). “For the first time, we have established that a single source of hESC can provide the multiple cell types needed to interact within a three-dimensional tissue model to generate complex, multilayer tissues. We are a step closer to a practical therapy to help with diseases of the skin and mouth,” Jonathan Garlick, DDS, PhD, says. He is an SDM professor of oral and maxillofacial pathology, and also an SSGBS Cell, Molecular & Developmental Biology Program faculty member.
“Researchers have been seeking methods to grow skin-like tissues outside of the body using new sources of stem cells such as hESC, with the goal of advancing regenerative medicine as a new therapy to replace or repair damaged or diseased tissue. Little is known about how hESC can be developed into the multilayer tissues similar to those that line the gums, cheeks, lips, and other areas in the mouth. We used in vitro tissue engineering techniques to produce skin-like tissues that mimic the lining tissues found in the oral cavity,” he goes on to explain.
In their research, the scientists used the (H9) cell line, which was grown in a combination of special chemical nutrients and specialized substrates. The resulting cells were made to differentiate into two separate types of mature cells – the epithelial tissue precursor ectodermal cells, and mesenchymal cells, the support layer underneath the former. These cells were then inserted into an engineered, air-liquid interface, which mimicked the environment of the oral cavity.
“These engineered tissues are remarkably similar to their human counterparts and can be used to address major concerns facing the field of stem cell biology that are related to their clinical use. We can now use these engineered tissues as 'tissue surrogates' to begin to predict how stable and safe hESC-derived cells will be after therapeutic transplantation. Our goal is to produce functional tissues to treat oral and skin conditions, like the early stages of cancer and inflammatory disease, as well as to accelerate the healing of recalcitrant wounds,” Garlick concludes.
 14 DAY TRIAL //
14 DAY TRIAL //