There are several kinds of diabetes, and it's hard to tell them apart considering that all of them are defined by high blood sugar levels over a prolonged period. Scientists from the Stanford University School of Medicine have found a way to accurately detect type-1 though.
Type-1 diabetes is an autoimmune disease that arises when an inappropriate immune-system attack is inflicted upon healthy tissues. As a consequence, the body stops producing insulin, a hormone that plays the greatest role in the processing of sugar. Specifically, a person's antibodies attack the insulin-producing cells in the pancreas.
The disease will lead to the appearance of auto-antibodies. Whether or not these antibodies are present lets medics know if it's type-1 or type-2 diabetes their patients are suffering from.
However, diagnosing the conditions can take too long. If treatment isn't administered to type-1 immediately, there might be unrepairable consequences in the long run.
Also, the normal test isn't exactly easy to pull off. Reliant on highly-trained laboratory staff and costing hundreds of dollars, it needs several days before a diagnosis can be given, since the blood and tissue samples are exposed to radioactive materials meant to detect the auto-antibodies.
The scientists from Stanford, however, were able to invent a chip that can do it in minutes, does not produce any radioactivity and can be used for 15 different tests. All the while costing only $20 / €15.
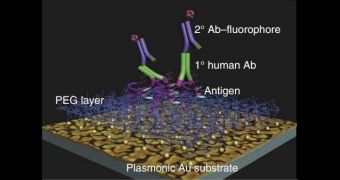
Instead of radioactive substances, the chip uses fluorescence to detect the antibodies. The secret lies in the nanoparticle-sized islands of gold coating the bases of each microchip. The gold intensifies the fluorescent signal of the auto-antibodies.
Moreover, this all can be done outside of hospital settings, which may just be as great an advantage as the cost effectiveness itself. The chips are meant to be used by handheld devices, so they could eventually become a standard instrument in medical field kits.
All that's left is for the Food and Drug Administration (FDA) to approve of the device and the world as we know it will change. Well, the world as medics and hospital staff know it anyway, but it is still a big change, both for specialists and for the people whose health is affected.
Especially the latter really. It's not at all unheard of for a misdiagnosis to happen, especially in people who possess more than one auto-antibody. And it wasn't that long ago that the different diabetes types were linked to ages (type-1 with children, type-2 with middle-aged overweight adults), but childhood obesity muddled those waters.
 14 DAY TRIAL //
14 DAY TRIAL //