The intricate interplay between various types of neurons that leads to the development of schizophrenia is currently the target of three separate labs at the University of Pennsylvania Perelman School of Medicine. In their latest report, the investigators say that sounds affect how the condition is triggered
In other words, the team discovered that the genetic risk factors for schizophrenia – which have been known for a rather long time – somehow interact with sound waves to trigger the disease in susceptible patient populations.
In order to arrive at this conclusion, investigators had to use a combination of numerous analysis techniques, including a special type of high-speed imaging, as well as electrophysiological, anatomical, and immunohistochemical techniques.
The lead author of the new study was Penn assistant professor of neuroscience in psychiatry Gregory Carlson, PhD. The US National Institutes of Mental Health (NIMH), a part of the National Institutes of Health (NIH), funded part of this investigation.
Results were detailed in the latest issue of the esteemed journal Proceedings of the National Academy of Sciences (PNAS), PsychCentral reports. The focus of the research was a protein called dysbindin, which was proven in past studies to play an important role in the development of schizophrenia.
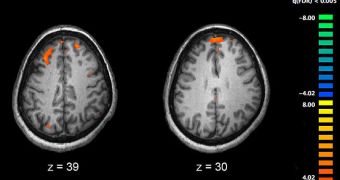
“Our work provides a model linking genetic risk factors for schizophrenia to a functional disruption in how the brain responds to sound, by identifying reduced activity in special nerve cells that are designed to make other cells in the brain work together at a very fast pace,” Carlson says.
“We know that in schizophrenia this ability is reduced, and now, knowing more about why this happens may help explain how loss of a protein called dysbindin leads to some symptoms of schizophrenia,” the team leader goes on to say.
Seeing that low dysbindin concentrations were tied to the development of this condition, the experts focused on analyzing the issue in more detail. The team created a lab mouse model of the disease, in which the rodents exhibited lower concentrations of this protein.
In the study, it was revealed that certain sound-processing areas in the mouse brain were being severely impaired by the low dysbindin levels. Neurons in those regions were shutting down in a way that also took down large volumes of other nerve cells.
The type of fast brain activity that the lack of this protein disrupts has been evidenced to be critical critical for short-term memory in humans. The team now plans to analyze the link in more detail.
 14 DAY TRIAL //
14 DAY TRIAL //