Schizophrenia and autism spectrum disorders (ASD), among other mental disorders, may be partially caused by insufficient concentrations of a protein called densin-180 in the brain. The new results were derived from studies carried out on lab mice.
While most mental diseases humans can develop are unique to our species, there are those that can affect animals such as rats and mice in similar patterns. They then start behaving in a manner similar to human patients; and researchers call these behaviors endophenotypes.
This is what researchers at the California Institute of Technology (Caltech) relied on when they devised their latest scientific study. They studied mice in which a gene was manipulated such that it no longer produced the densin protein.
In the absence of this molecule, the lab animals began displaying endophenotypes that past studies have associated with schizophrenia and ASD, among others. Details of the study appeared in a recent issue of the esteemed medical Journal of Neuroscience.
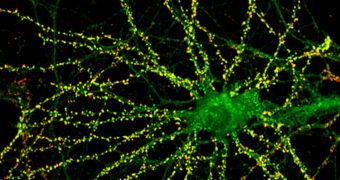
The senior author of the paper was the Caltech Allen and Lenabelle Davis professor of biology, Mary Kennedy. She explains that the target protein is usually very abundant inside synapses, the connections binding individual nerve cells in the brain together.
The most important role that densin plays in synapses is to facilitate the communications between several other proteins, which are also key to achieving optimal data transmission between neurons.
“Our work indicates that densin-180 helps to hold together a key piece of regulatory machinery in the postsynaptic part of excitatory brain synapses,” Kennedy explains. Without it, several other regulatory proteins – including one called DISC1 – became available only in limited amounts.
“A mutation that leads to loss of DISC1 function has been shown to predispose humans to development of schizophrenia and bipolar disorder,” the team leader adds. The study therefore indicates that a new avenue for research in treating these conditions may now lay open before researchers.
Scientists now plan to conduct additional studies to determine the exact mechanisms through which reduced regulatory protein concentrations in synapses lead to behavioral endophenotypes in animals.
The next step will be to test and see whether similar mechanisms exist in the human brain. If that turns out to be the case, then it may become possible to develop new protein-based therapies based on those findings.
“The molecular mechanistic links between a gene defect and defective behavior are complicated and, as yet, mostly unknown. Understanding them goes to the very heart of understanding brain function,” Kennedy concludes.
 14 DAY TRIAL //
14 DAY TRIAL //