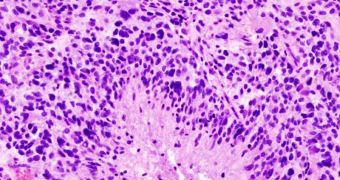
According to a study conducted by researchers at the Northwestern University, a new type of gene therapy has proven effective in increasing survivability among animals suffering from glioblastoma.
This research could mark a significant progress in the fight against one of the most aggressive and fast brain cancers in the world. This condition moves extremely quick and is incurable.
Statistics from the National Institutes of Health suggest that glioblastoma multiforme (GBM) is responsible for more than 13,000 deaths in the United States every year.
The new study could contribute to reducing this number in the future. Experts focused on demonstrating a new delivery system for a drug that targets one of the essential genes the cancer needs in order to develop properly.
One of the main challenges associated with treating brain cancers is that many of the chemical agents included in drugs cannot pass through the blood-brain barrier, a defense mechanism that filters out any potential pathogens from the blood before it enters the brain.
NU experts were able to avoid this issue by turning to nanotechnology, thus ensuring that all active ingredients reach their destination.
The target gene was discovered in 2007 by a team of experts including Alexander H. Stegh, who lead this research with the NU George B. Rathmann Professor of Chemistry Chad A. Mirkin, a senior co-author on the study.
Called Bcl2Like12, the gene plays an important role in conferring GBM an increased level of resistance to conventional therapies. With the new approach, drugs delivered intravenously can enter the cancer cells, and simply switch off the troublesome gene, thus knocking out all the proteins that the former encodes.
In a study conducted on mice, survivability rates increased nearly 20 percent, while the size of the GBM tumors decreased, on average, between 300 and 400 percent. Details of the study appear in the October 30 issue of the journal Science Translational Medicine.
“This is a beautiful marriage of a new technology with the genes of a terrible disease. Using highly adaptable spherical nucleic acids, we specifically targeted a gene associated with GBM and turned it off in vivo. This proof-of-concept further establishes a broad platform for treating a wide range of diseases, from lung and colon cancers to rheumatoid arthritis and psoriasis,” Mirkin explains. He adds that the next step in the research is moving to human clinical trials.
If the work proves successful, this study could mark a turning point in the way oncologists battle this highly aggressive form of cancer. Additionally, the approach could potentially be extended to cover other common types of cancer.
 14 DAY TRIAL //
14 DAY TRIAL //