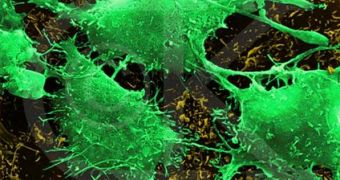
Experts from the Harvard Medical School (HMS) Massachusetts General Hospital (MGH) have managed to discover a new biomarker that holds the potential to allow doctors to more accurately identify patients with recurrent glioblastoma (brain tumors), who could potentially respond to anti-vascular endothelial growth factor therapy. The researchers took the cediranib therapy as an example. In this form of treatment, cediranib effectively inhibits the vascular endothelial growth factor (VEGF) receptor tyrosine kinases.
According to the research team, when patients were given the cediranib pill, special forms of magnetic resonance imaging (MRI) revealed immediately, since the first dose, if the drug had any effect on them or not. This type of immediate response could be very useful in emergency situations, when health-care professionals need to determine quickly what type of therapy is best suited for their patient.
“We found that results from an advanced MRI scan taken just a day after starting treatment correlated with survival. Combining MRI with blood biomarkers did an even better job of identifying patients who best responded to treatment. If this approach is validated in larger studies, we could use these tools to keep patients on therapies that their tumors respond to, and shift non-responders to other therapies much earlier,” HMS Associate Professor of Radiology and Health Sciences and Technology A. Gregory Sorensen, M.D., who has also been one of the main researchers in the new study, explained.
The key element the MRI scans were looking for was vascular normalization. Once this occurred, it was then clear for the researchers that the new drug had worked. Some 31 patients with recurring brain tumors were analyzed, one day prior, and one day after they took the cediranib pill. “Vascular normalization is an important mechanism of how these drugs work in cancer patients,” HMS Andrew Werk Cook Professor of Tumor Biology Rakesh K. Jain, PhD, who is also the director of the Edwin L. Steele Laboratory for Tumor Biology at the department of radiation oncology, MGH Cancer Center, added.
“I was intrigued by the findings from this innovative trial, especially the fact that you could use separate biomarkers in combination to potentially predict the outcomes of patients. This is really a severe disease and being able to determine response at such an early point is helpful to tailor treatment. If we can predict those responding to antiangiogenic therapy early on, we may be able to define where the benefit would be,” the Deputy Editor of the journal Cancer Research, Richard B. Gaynor, M.D., PhD, concluded. The journal published the new study in its latest issue.
 14 DAY TRIAL //
14 DAY TRIAL //