Researchers at the Stanford University have just demonstrated that it's possible to convert adult human skin cells directly into working nerve cells called neurons. Furthermore, this can be done without the need to first turn them into induced pluripotent stem (iPS) cells.
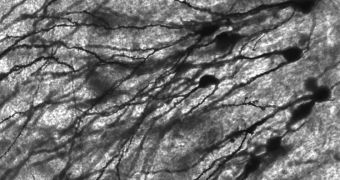
Stanford School of Medicine experts managed to do this by adding just four proteins to a population of adult skin cells. Within 4 to 5 weeks, all of the cells were turned into functional neurons. The latter are critical for the transmission of electrical impulses in the brain.
Without having to pass through an iPS stage, new neurons can now be tailored for individual patients or specific diseases much easier than before. The technological process to create them was simplified considerably as well.
An added advantage in avoiding iPS cells is that the issues detected with these types of cells recently will no longer influence the overall result of the conversion process. In studies conducted on lab animals, the bodies of mice rejected iPS cells derived from their own adult cells.
“We are now much closer to being able to mimic brain or neurological diseases in the laboratory. We may perhaps even be able to one day use these cells for human therapies,” says Marius Wernig, MD.
The expert, a member of the Stanford Institute for Stem Cell Biology and Regenerative Medicine, holds an appointment as an assistant professor of pathology at the university. He is also the senior author of a new study detailing the findings.
Details of the research appear in the May 26 online issue of the top journal Nature.
In order to achieve a successful conversion, experts had to use a cocktail of four proteins called transcription factors. The mix included Brn2, Ascl1 and Myt1l (BAM), plus the moelcule NeuroD.
“The iPS cell approach is doable and has been shown to work. We need to keep working on both strategies. It’s possible that the best approach may vary depending on the disease or the type of research being done,” Wernig explains.
The study was supported by grants from the Stanford Institute for Stem Cell Biology and Regenerative Medicine, the Ellison Medical Foundation, the Stinehard-Reed Foundation, the Donald E. and Delia B. Baxter Foundation, the New York Stem Cell Foundation and the National Institutes of Health (NIH).
 14 DAY TRIAL //
14 DAY TRIAL //