A group of investigators from the Massachusetts General Hospital (MGH) in Boston determined in a new study that missing gut bacteria appear to play a very important role in the development and progression of Crohn's disease, an inflammatory bowel disorder also known as regional enteritis.
The research focused on around 1,500 test subjects diagnosed with this disease and found that most of these individuals had less diverse gut flora than their healthy peers. This study marks the first time that bacterial changes are identified in Crohn's disease patients, potentially highlighting new avenues of research for developing a more effective course of treatment.
MGH investigator and study leader Ramnik Xavier says that nearly one million people are suffering from this IBD in the United States alone. The disease is characterized by pain, bleeding, diarrhea, and weight loss, usually triggered at first by an over-active immune system. Other symptoms are manifested, too.
One of the most common courses of treatment at this point is steroids, which patients have to take regularly. In addition to causing some pretty severe side-effects, these compounds also have the disadvantage that they might not actually work in correcting the issue. As such, surgeons oftentimes have to remove portions of the digestive tract in patients to stem the progression of the disease.
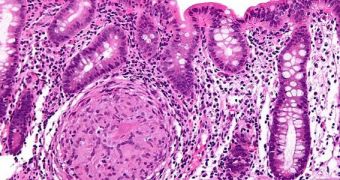
In the study, gut flora samples from 447 Crohn's disease patients were compared to samples collected from 221 healthy individuals. What was made immediately obvious was that people in the first group had a mix of digestive tract bacteria that were more likely to excite the immune system, accounting for the overreaction doctors see when the condition is first triggered.
Details of the research paper were published in the latest issue of the esteemed scientific journal Cell, Host and Microbe. The team says that patients also tend to have more bacteria that promote inflammation than bacteria that stop it, which also contributes to explaining the behavior of the human immune system in this condition.
One of the most worrying conclusions of the research was that children whose doctors had prescribed antibiotics before Crohn's was accurately diagnosed fared the worst. “We may have to revisit the use of antibiotics in [these] patients with early-onset Crohn's disease,” Xavier explains, quoted by NPR.
The new study suggests that researchers could try their hand at developing so-called super-probiotics, medication that promotes the selective growth of only beneficial bacteria in the intestinal flora. This could enable Crohn's patients to withstand the immune assault much better, and it could even diminish its intensity to some extent.
By learning to tweak gut flora rather than bashing it over the head with antibiotics, a wide array of conditions related to the actions of the immune system – which are often controlled by the gut – might find new cures, experts comment.
 14 DAY TRIAL //
14 DAY TRIAL //