The hormone insulin is essential for the human body. One of its primary roles is to convert sugars, starches, and other types of food into energy for the entire organism. However, the cells that produce them, called beta-cells and located in the pancreas, can be hindered at times. When this happens, diabetes type I ensues. The condition is more commonly found in children, but instances when it was discovered in adults were also recorded. The condition is also known as juvenile diabetes, and it can have significant implications for a patient's health, AlphaGalileo reports.
The affliction develops when the beta-cells in the human pancreas come under attack from an autoimmune mechanism, which methodically destroys them. Insulin levels in the blood drop sharply, and a number of severe side-effects can develop. The only way to treat the disease is to inject insulin daily. However, this approach is cumbersome, time-consuming, and prone to all manner of side-effects as well, such as gangrene, blindness, and kidney failure. In a new study, researchers wanted to determine whether the beta-cells could still reproduce when nearly wiped out by the immune system.
Detecting the regeneration process is a very difficult task, simply because it may be overshadowed by the destruction of beta-cells going on at the exact same time. “We wanted to study the capacity of the pancreas to produce new beta-cells after their near-total loss, a condition close to Type 1 diabetes, but without autoimmunity,” says University of Geneva (UNIGE) Faculty of medicine professor Pedro Herrera. He is also a member of the Swiss Frontiers in Genetics program. The scientist led a team of colleagues in creating transgenic mice, animals especially modified to exhibit the genetic traits the investigators wanted to study.
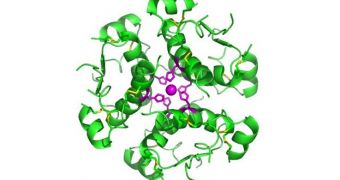
In the mice study, the team determined that even rodents which experienced massive beta-cell loss were able to grow their insulin-producing structures back, oftentimes through unexpected mechanisms. “We were surprised to find that production of new beta-cells results mainly from the spontaneous conversion of a completely different type of cells, the so-called alpha-cells. The latter are indeed programmed to synthesize glucagon, a hormone whose function is opposite to that of insulin,” the group leader says.
“Whether this is the consequence of a continuous regeneration of new beta-cells, as we have seen in mice, or persistence of few beta-cells, which have escaped autoimmunity, is not known,” explains the first author of the new investigation, UNIGE expert Fabrizio Thorel. “The amount of beta-cell destruction thus appears to determine whether regeneration occurs. Moreover, it influences the degree of cell plasticity and regenerative resources of the pancreas in adult organisms,” Herrera concludes.
 14 DAY TRIAL //
14 DAY TRIAL //