Scientists from the University of Southern California (USC), led by associate professor of biomedical and electrical engineering Ellis Meng, are currently working on developing a new type of miniaturized, implantable drug infusion pump, which will help oncologists treat an aggressive type of brain cancer called leptomeningeal metastases in pediatric patients.
This condition is extremely severe in all age groups, but becomes even more so in children. At the same time, treating children is a daunting task, since their bodies are not yet capable of taking the amount of beating that the adult body can.
Treating brain cancers of any types is further complicated by the blood-brain barrier (BBB), a series of filters that clean out all foreign chemicals from the blood, before the latter is allowed to irrigate the brain. In order to circumvent this defense mechanism, the USC team develops the new pump.
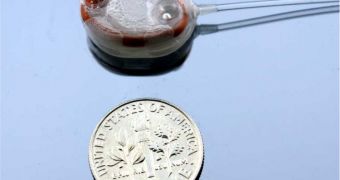
Roughly the size of two small cookies stacked on top of each other, the pump is capable of releasing small amounts of the necessary drugs over prolonged periods of time. The research is being conducted with funds from the US National Science Foundation (NSF).
Meng has already started a new enterprise called Fluid Synchrony LLC, whose purpose is to promote the use of these high-efficiency miniature pumps in clinical and human trials. The researcher already has 6 patents for the technology, with another dozen or so awaiting approval.
Leptomeningeal metastases works by affecting the lining of the brain and spinal cord, so the drug pump would be installed in the abdomen, and made to deliver chemotherapy drugs directly into the spinal cord. This would ensure that the drugs are sent directly into the brain, bypassing the BBB entirely.
“With this disease, you need a lot of drug, since the spinal fluid is constantly being made and replenished, every six hours. So it makes sense to treat with this type of pump, because we have the ability to dose frequently,” Meng explains.
“We use a simple technique to electronically control how much drug is pumped, when it is pumped and how often it is pumped,” the researcher adds. An added benefit of these pumps is that they are self-powered, meaning that patients using it will not be tied down to their beds.
Meng says that this is very important for morale, as cancer patients hate to be constantly reminded of their condition. “The idea is to avoid frequent trips to the doctors for these injections, which can be traumatic. You put the implant in the eye wall, and it continues to dispense the drug until it runs out. The only thing you have to do is get the device refilled,” the team leader concludes.
 14 DAY TRIAL //
14 DAY TRIAL //