At this time, HIV-positive women are asked to take Pap smears at very regular intervals, significantly more often than their HIV-negative peers. Following a new study, scientists determined that the frequency of such tests can be reduced via a new approach.
Following a study conducted on 420 HIV-positive and 279 HIV-negative women, researchers at the Yeshiva University Albert Einstein College of Medicine (AECM) found that combining Pap smears with HPV screenings can efficiently predict the incidence of cervical cancer in both groups.
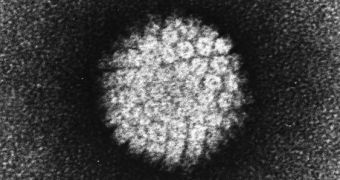
Until now, the thinking among doctors has been that HIV infections and AIDS boost women's chances of developing cervical cancer, because of the fact that these conditions suppress the immune system. Since cervical cancer is caused by the Human Papilloma Virus (HPV), the connection was obvious.
However, AECM investigators say that women who suffer from HIV infections don't need to undergo very frequent Pap tests. All the participants in the new study were enrolled in the Women's Interagency HIV Study (WIHS), Science Daily reports.
The findings were presented at a JAMA media briefing at the International AIDS Conference, on July 22. The presentation was held by AECM professor of epidemiology and population health, Howard Strickler, MD, MPH.
Results will also be published in the July 25 issue of the esteemed Journal of the American Medical Association (JAMA). The team believes that combining Pap and HPV screenings could significantly improve quality of life for HIV-positive women, and reduce the number of biopsies they undergo.
This will come in handy for the ~1.2 million people who suffer from HIV in the United States alone. These figures belong to official statistics from the US Centers for Disease Control and Prevention (CDC), published in 2009 and covering people over the age of 13.
“It is widely thought that before cervical precancer or cervical cancer can develop, there must be persistent infection by a cancer-associated HPV, as well as the accumulation of additional genetic changes over time,” says Dr. Strickler, who is also the senior author of the JAMA paper.
“Overall, few cases of cervical precancer would have gone undiagnosed if the HIV-positive women did not have any additional Pap tests during the five years following enrollment -- no more than in the HIV-negative group,” lead author and AECM associate professor of medicine, Marla Keller, MD, adds.
“Thus, these data raise the possibility that HPV and Pap co-testing could be used to reduce the burden of frequent Pap tests and, by extension, unnecessary biopsies in HIV-positive women who are in long-term clinical follow-up,” she concludes.
 14 DAY TRIAL //
14 DAY TRIAL //