According to the conclusions of a new scientific study, it would appear that removing another 2 millimeters of tissue from the area surrounding a breast cancer tumor can substantially reduce the risk of residual disease setting in.
The approach works especially well with invasive forms of the disease, say experts from the Department of Breast Surgery at the Good Hope Hospital, in Sutton Coldfield, the United Kingdom.
Surgeons at the Hospital investigated the cases of more than 300 women, who got breast cancer surgery at the facility between 2002 and 2008.
Full details of their investigation appear in the November issue of the International Journal of Clinical Practice (IJCP), AlphaGalileo reports.
“Breast conserving surgery followed by radiotherapy is a well-established alternative to breast removal and studies have demonstrated similar survival rates in patients undergoing these procedures,” says Dr Stephen Ward.
The expert was also the lead author of the new study. “However patients undergoing breast conserving surgery are more likely to have recurrent cancer and the amount of tissue removed around the tumor,” he adds.
“A survey of 200 UK breast surgeons published in 2007 revealed wide variations in what they considered to be an adequate margin, with 24% wanting a clear margin of 1mm and 65% wanting a margin of 2mm or more,” he explains.
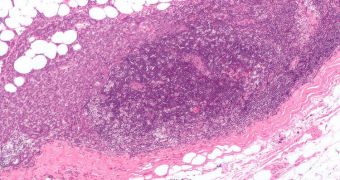
The investigation revealed that only 2 percent of women who had received the new type of surgery showed signs of residual disease, defined as the presence of invading or non-invading cancer cells.
For comparison, some 35.3 percent of women who didn't have the extra tissue removed showed signs of residual disease.
“Our research found that the overall probability of finding residual disease was 2.4% if a woman had surgery where the free margin was 2mm or more from the invasive cancer,” Ward explains.
“But the same pattern was not observed when the woman had surgery for non-invasive cancer, where the incidence of residual disease was higher,” he adds.
The expert goes on to say that the new procedure should be applied on a much larger scale in instances when invasive cancer is detected.
As for the cases where non-invasive, localized forms of the disease are present, the correlation was less clear, and the surgeon team argues that more investigations are needed into the issue.
 14 DAY TRIAL //
14 DAY TRIAL //