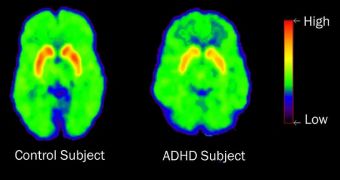
According to a team of scientists at the Washington University in St. Louis (WUSL) School of Medicine (WUSM), common types of brain scans could be used to assess whether drugs designed to fight attention deficit hyperactivity disorders are causing high dopamine concentrations in the brain.
If that is the case, then the drugs could be used to treat a variety of other mental conditions that feature an inattentiveness, and the inability to properly concentrate on the task at hand. One such disorder is called neurofibromatosis type 1 (NF1), and it affects more than 100,000 people in the United States.
Official statistics indicate that anywhere from 60 to 80 percent of all people suffering from this disorder exhibit attention deficit symptoms, similar to those displayed by ADHD patients. In a previous study, the team determined that elevated dopamine levels improved attention in NF1 patients.
If they are able to demonstrate that the ADHD medication has the same effect in the brains of ADHD patients, then it may be possible to prescribe the aforementioned drugs to NF1 patients as well.
In fact, what the researchers are really interested in is figuring out the differences in the brain that cause the development of either ADHD, NF1, or other attention-deficit disorders. If the mechanisms are proven to be the same, then there would be no problem in treating all patients the same.
“Many kids with NF1 really struggle in school, and finding ways to help alleviate attention problems is a high priority,” explains the WUSM Donald O. Schnuck Family Professor of Neurology, David H. Gutmann, MD, PhD,” quoted by PsychCentral.
“The technique we’ve refined may make it possible to match specific treatments to the patients with NF1 and attention deficit who are most likely to benefit from those treatments,” he goes on to say.
“This mouse model may not be a perfect model for all forms of attention deficit, but it is a terrific model for one type of attention system dysfunction. Greater understanding of what goes wrong in some children with NF1 could lead to new insights into a broader variety of attention problems,” he adds.
The investigator also holds an appointment as the director of the Washington University Neurofibromatosis (NF) Center. Together with other experts in his group, he genetically manipulated mice to create models of the NF1 brain, as well as neural tumors.
In a previous study, the same team demonstrated that mice who were given Ritalin had a tendency to exhibit normal dopamine levels, if they previously lacked them. The common ADHD drug was also able to cure the little rodents of their inattentiveness.
“This finding suggested that raclopride PET imaging could be used as a platform for preclinical testing of drugs that may affect brain dopamine levels. We can get an image in an hour and assess the effects of the drug on mouse behavior in a day,” Gutmann says.
“As we learn more about the different ways attention deficits arise in these children, it may be possible to use the prescreening data and preclinical drug tests in mouse models to select the best drug for each patient,” he concludes.
 14 DAY TRIAL //
14 DAY TRIAL //