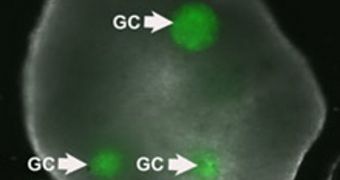
Using tissue engineering and other biotechnology methods, a team of researchers in the United States has developed the first entirely-artificial human ovary.
The synthetic organ was developed so that women looking to have children, but who are infertile, can do so. This major breakthrough was achieved at the Brown University, Technology Review reports.
One day, the researchers behind the new work hope, the tissue engineering methods used to create this construct will be used to mature human eggs, bringing the goal of artificial reproduction a lot closer.
But, for now, the artificial ovary has numerous practical applications of great importance. For example, it could be used to develop new contraceptive medication.
Assessing the impact that toxins and other chemical in women's daily environments have on their ovaries will also become easier, as will the study of fertility-enhancing substances.
Additionally, oncologists may have just got a new tool for studying ovarian cancer. They could look at how the disease develops and progresses without actually needing sick subjects.
In a new paper detailing the discovery, that appears in the current issue of the esteemed Journal of Assisted Reproduction and Genetics, researchers show that the new ovary could also conceivably be used to mitigate the effects of illness, radiation and chemotherapy on women.
“The concept of creating an artificial three-dimensional environment, and the fact that we can take out immature eggs and let them grow and mature into viable eggs, is really exciting,” says the director of infertility at Mt. Sinai Medical Center in New York, Alan B. Copperman
The expert, who was not involved in the work, says that though many challenges remain ahead, the Brown team has demonstrated immense potential with this work.
“If we can establish a viable testing environment, we can learn more about how to optimize eggs, and discriminate good from bad eggs,” Copperman goes on to say.
The research group now plans to investigate the mechanisms promoting egg cell maturation in greater detail. Experts already suspect some proteins of playing a great role, but this has yet to be accurately established.
“We could also theoretically find something that might be important in the development of ovarian cancer. We're not there yet, but I think this is going to be the most powerful use of the model,” explains expert Sandra Carson.
She was the lead researcher on the new investigation. Carson is also a professor of obstetrics and gynecology at the Brown University, and also holds an appointment at the Woman and Infants Hospital of Rhode Island.
 14 DAY TRIAL //
14 DAY TRIAL //